Long-Covid & Chronic Illness
Long-Covid
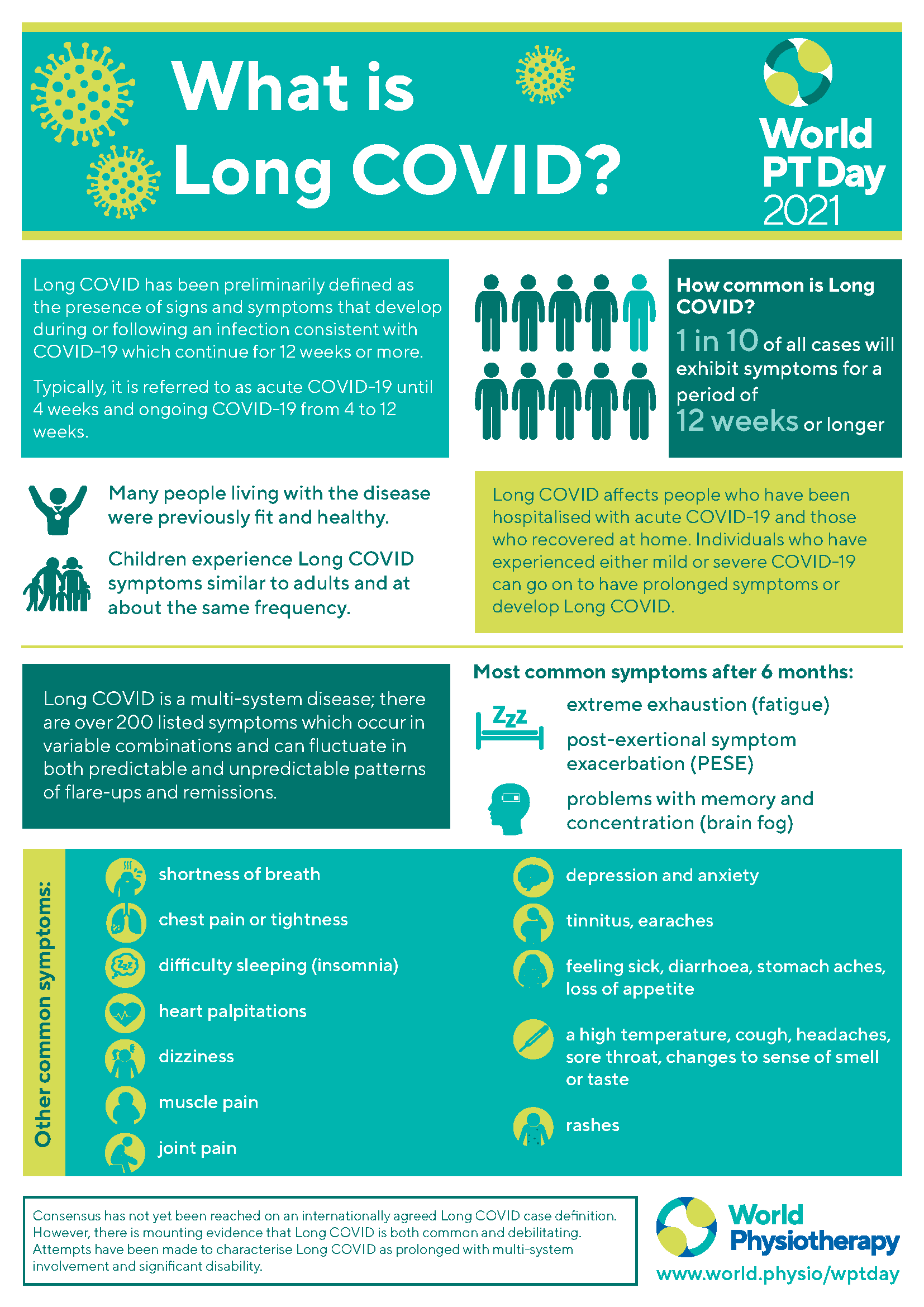
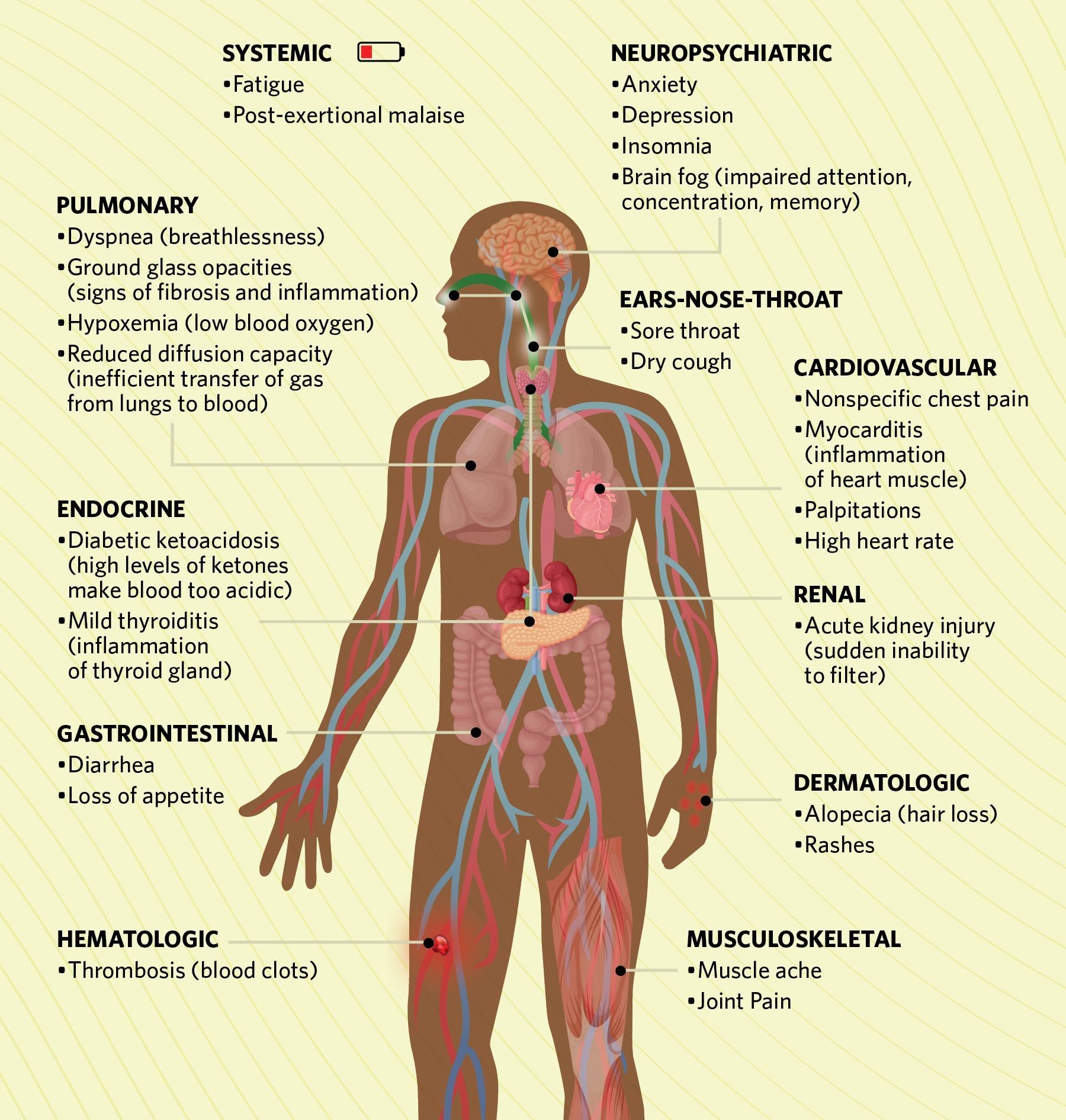
Long COVID, also known as PASC - Post-Acute Sequelae of SARS-CoV-2, is a complex, multi-system, post-viral condition that develops after an initial COVID-19 infection. Symptoms persist for at least 12 weeks after infection and can affect nearly every system in the body. Conservative estimates suggest that up to 20% of people who contract COVID-19 may develop Long COVID, with over 200 reported symptoms. These symptoms often present in varying combinations and may fluctuate in both predictable and unpredictable cycles of flare-ups and remissions.
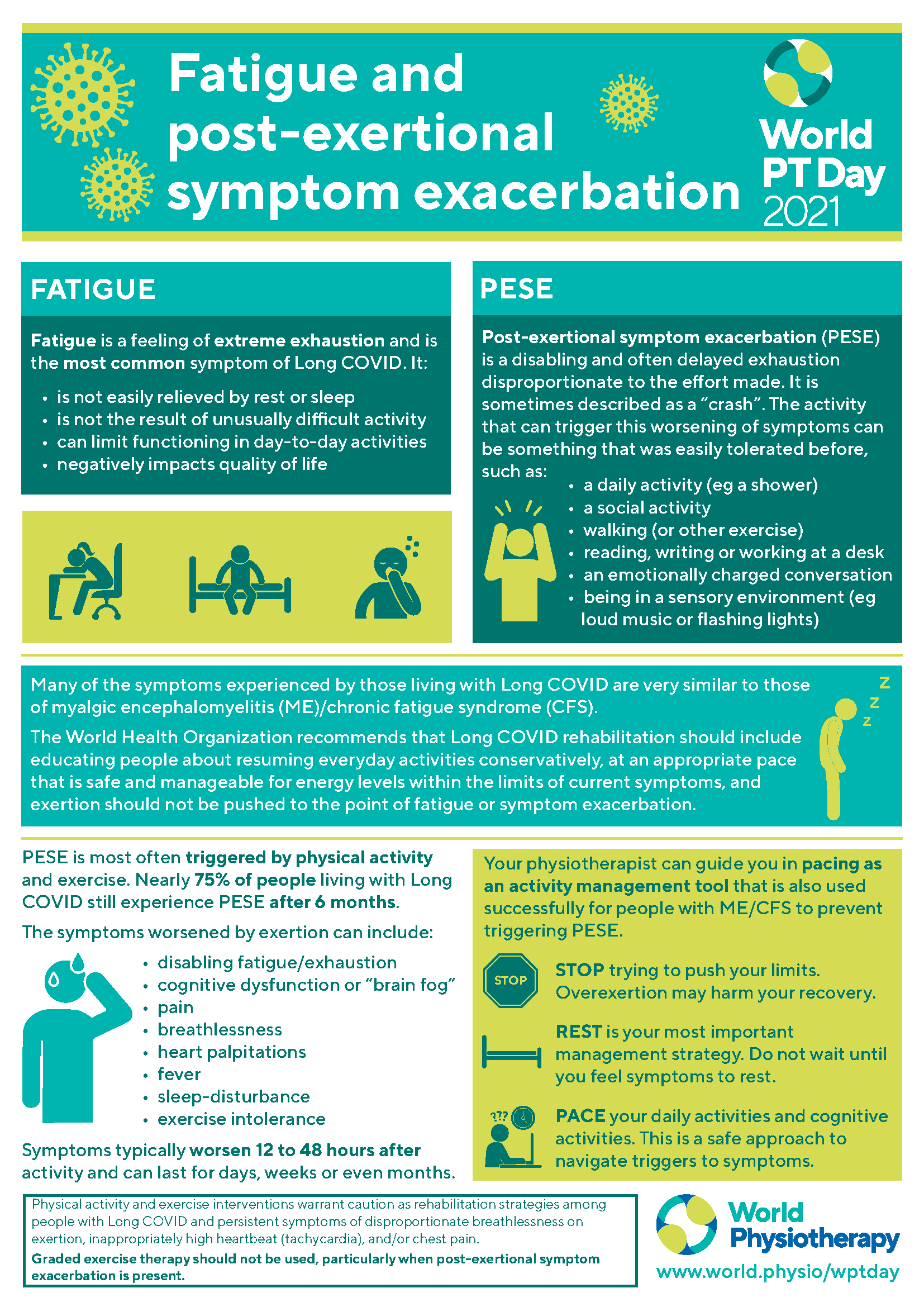
Among the most common symptoms are fatigue, brain fog, post-exertional malaise (PEM) and shortness of breath. Mental health is also significantly impacted, with many individuals experiencing anxiety, depression and PTSD as a result of their condition and the losses that come with it.
If you’ve been diagnosed with Long COVID, or suspect you may be living with it, I would be honored to support you. Our work together will focus on making sense of your experience, grieving the loss of your pre-illness functioning and navigating the many challenges that come with chronic, often misunderstood illness.
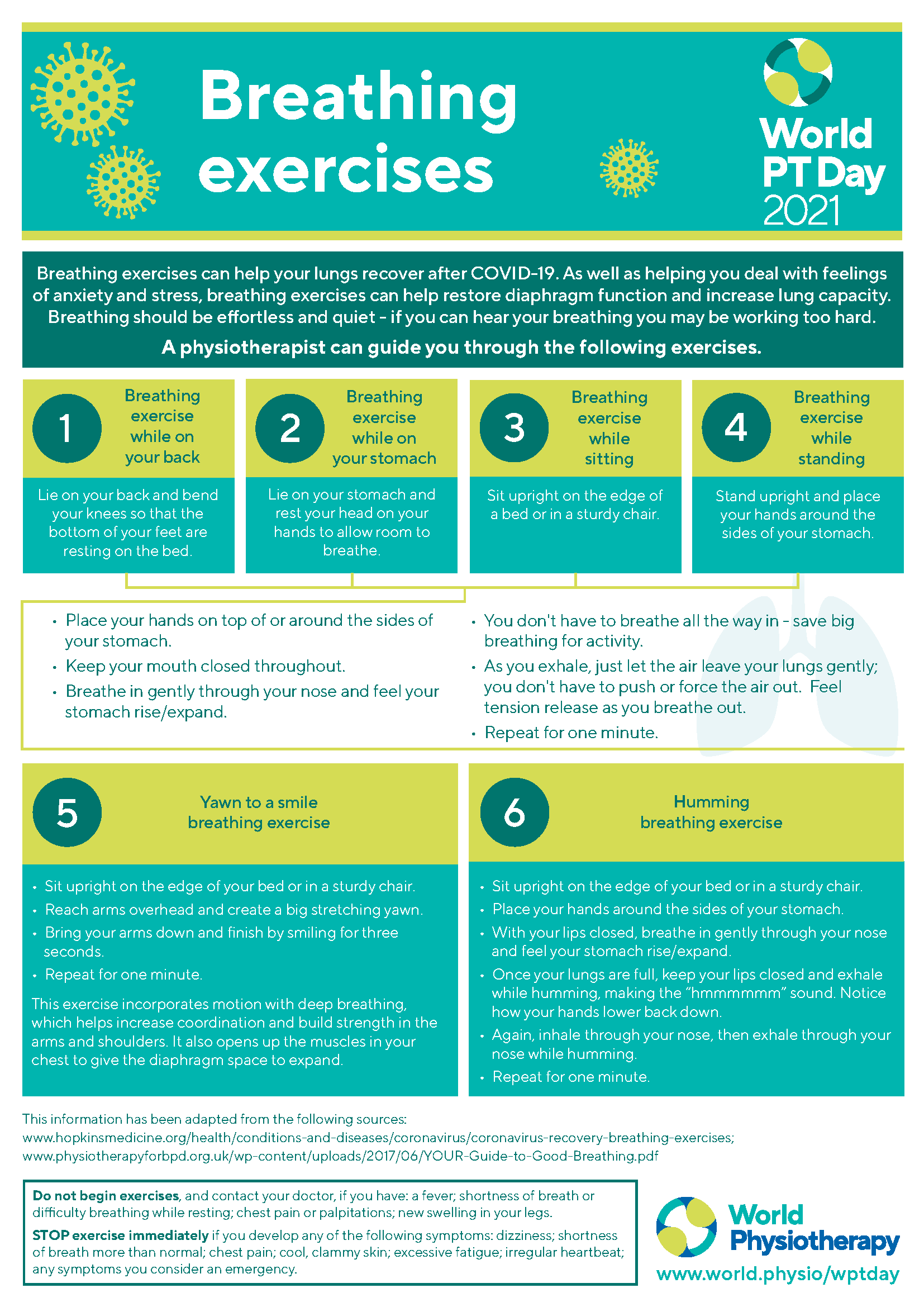
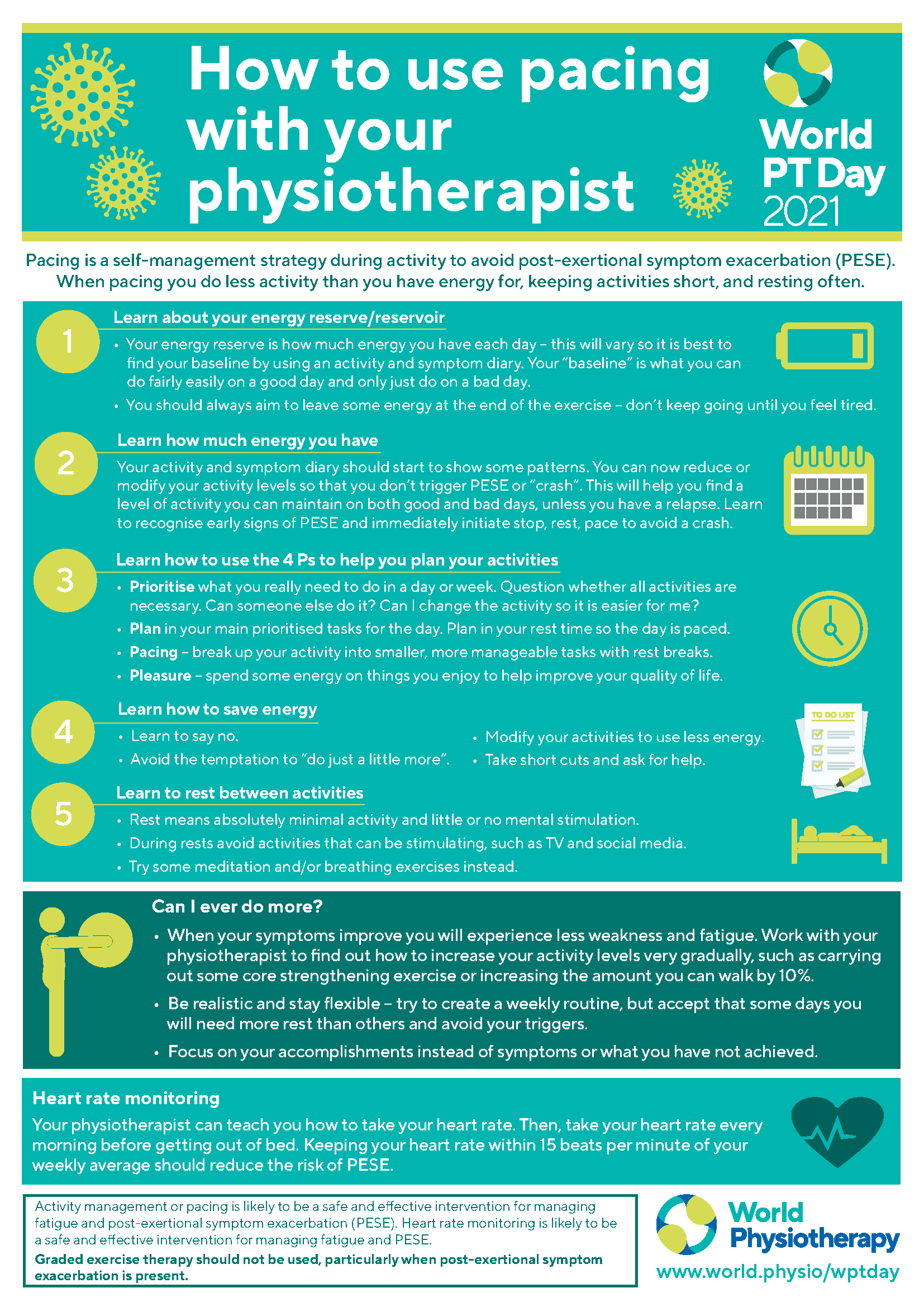
We’ll explore how to support your nervous system, honor your body’s current capacity, and shift from traditional goal-setting to celebrating small, meaningful wins. Our work will also include learning how to engage with the medical system in ways that protect your emotional well-being and avoid additional trauma. I can provide practical tools and resources to help track symptoms, manage daily functioning and explore treatment options with greater clarity and confidence.
Chronic Illness
If you’ve been newly diagnosed, or have been living with a chronic health condition for years, you have felt the impact of the illness on your mental health. Whether you have fibromyalgia, IBS, endometriosis, hypermobility, cancer, PCOS, a thyroid condition or any other chronic health issue, our work together to address the SIX NEEDS OF MOURNING (Wolfelt & Wolfelt, 2019):
Acknowledging the reality of your diagnosis and prognosis
Embracing the pain of your losses
Remembering your past
Incorporating your illness into your self-identity
Searching for meaning
Receiving ongoing support from others
As a person who’s lived with chronic health conditions, I’m in a unique position to help you work through your thoughts, emotions and experiences with chronic illness. I will always affirm your experience of your health and help you to navigate the complicated health care system, as well as explore alternative treatment methods you feel might be supportive. Together we will create a cohesive narrative of your health and your future.
My Long-Covid Story
I contracted COVID-19 in April 2022. After two years of diligently masking and limiting my activities to avoid the virus, I let my guard down during a trip. My acute infection lasted about a month, with the first two weeks marked by severe fatigue, migraines, brain fog, malaise, sore throat, muscle weakness, joint pain, congestion, shortness of breath and dizziness. I was fortunate to have been vaccinated and double-boosted, and I had access to two 5-day courses of the antiviral Paxlovid.
However, even after the acute phase passed, I never fully recovered. Early on, I was guided by a dear friend, a fellow Long Hauler whom I affectionately call my “Long Covid doula” (a term she coined), who taught me that rest and early intervention were crucial to any hope of recovery. Since then, I have explored many treatments, including acupuncture, osteopathic manipulation, craniosacral therapy, heart rate variability biofeedback, the Safe and Sound Protocol, nervous system regulation skills, supplementation, dietary changes and more.
In July 2022, I was admitted to the now-closed Long Covid Clinic at Scripps Mercy Hospital. From there, I was referred to the Brain Injury Recovery Program at Scripps, where I worked for two months with an occupational therapist, speech and language pathologist, and neuro-physical therapist to address my Long Covid-related limitations.
These treatments have led to important discoveries about my health and have significantly reduced my fatigue, brain fog, post-exertional malaise, and symptoms of depression and anxiety. While I’m not yet fully recovered, I have learned to recognize my limits and pace myself accordingly. It is through these experiences that I developed a passion for supporting others navigating this difficult journey and helping them find their way back to themselves.
Update as of June 2024: Earlier in the year, I underwent surgery for endometriosis. Post-operatively, my care team and I began to explore the idea that inflammation from endometriosis was exacerbating my Long COVID symptoms. The surgery was very successful, and by addressing this root cause of inflammation, my symptoms have dramatically improved. While not everyone is able to identify the root cause of their Long COVID, I feel incredibly grateful to have found mine and to greatly reduce my symptoms.